Whether you are a professional athlete, a weekend runner, or someone passionate about fitness, performing at your best requires more than just training hard. It demands proper recovery, injury prevention, and body optimisation.
Sports physiotherapy is not only about treating injuries after they occur; it’s about maximising performance, preventing setbacks, and ensuring your body can consistently meet the demands of your sport. With millions of athletes worldwide turning to physiotherapy, research and experience both confirm that it plays a vital role in enhancing sports performance.
In this guide, we’ll explore the advantages of sports physiotherapy, how it works, the science behind it, and why every athlete, from beginners to elite performers, should make it part of their training routine.
Understanding Sports Physiotherapy
Sports physiotherapy is a specialised branch of physiotherapy that focuses on:
- Injury prevention – Reducing risks by addressing weak points in the body
- Rehabilitation – Helping athletes recover from sports-related injuries
- Performance optimisation – Enhancing strength, flexibility, and endurance
- Education and training – Teaching proper movement patterns and recovery strategies
Sports physiotherapists work closely with athletes, coaches, and doctors to design individualised programs that match the unique physical demands of a sport.
Why Sports Physiotherapy is Essential for Athletes
1. Injury Prevention—The Foundation of Longevity in Sports
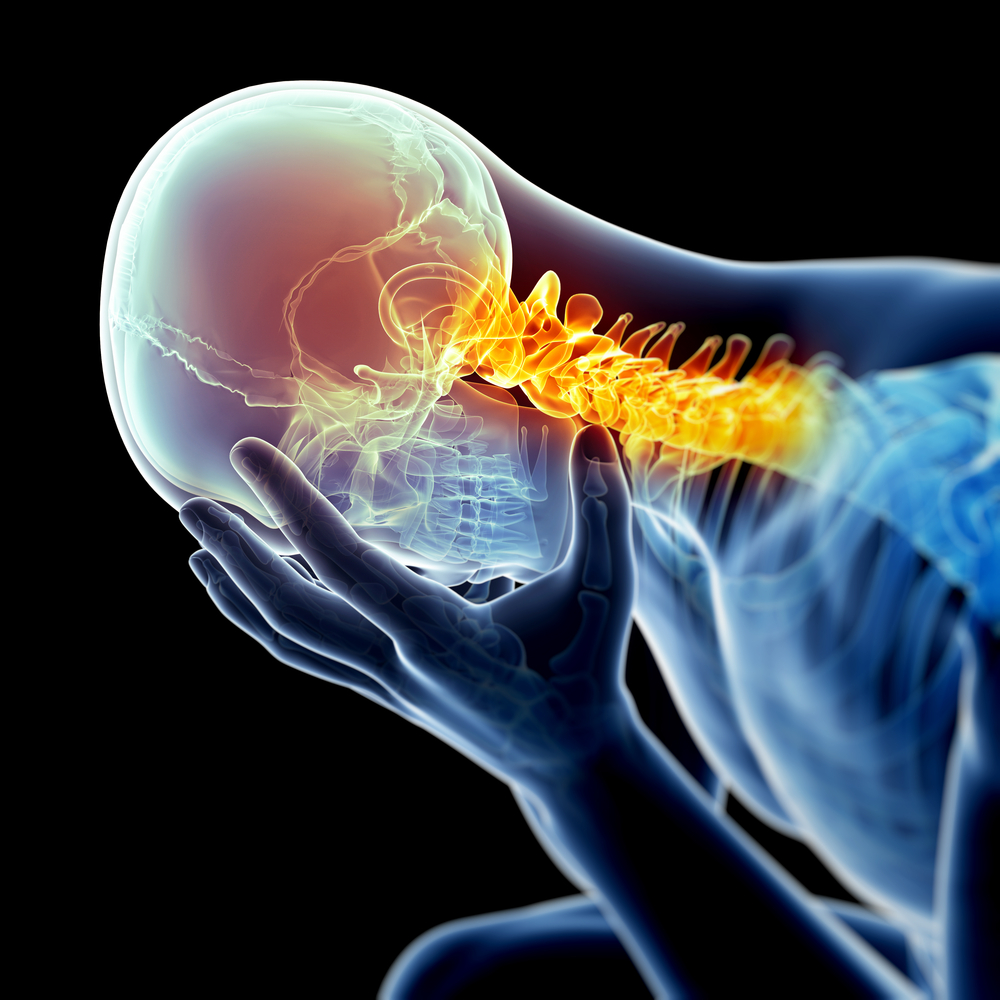
Injuries are the biggest barriers to consistent athletic performance. Sports physiotherapists analyse biomechanics, muscle imbalances, and joint stability to identify potential risks before they turn into injuries.
How it helps:
- Customised warm-up and cool-down routines
- Strengthening weak muscle groups
- Correcting poor posture or movement mechanics
Example: Runners prone to shin splints benefit from targeted calf strengthening and gait retraining, reducing recurrence significantly.
2. Faster Recovery from Sports Injuries
Despite precautions, injuries are part of sports. Physiotherapy accelerates healing by combining manual therapy, guided exercises, and advanced modalities like ultrasound or electrical stimulation.
Key recoveries supported by sports physiotherapy:
- Ankle sprains
- ACL (knee ligament) injuries
- Shoulder impingement
- Hamstring strains
Advantage: Faster return-to-play with reduced risk of re-injury.
3. Enhancing Flexibility and Range of Motion
Limited flexibility can compromise performance and increase the risk of injury. Sports physiotherapists use stretching techniques, mobility drills, and myofascial release to improve flexibility.
4. Improving Strength and Conditioning
Physiotherapists design strength training plans that go beyond general gym workouts. These programs target specific muscle groups that support athletic performance.
Example: For footballers, physiotherapy emphasises hamstring and hip strengthening to improve sprint speed and reduce muscle tears.
5. Optimising Movement and Technique
Sports performance depends heavily on proper biomechanics. Physiotherapists use video analysis and movement assessments to identify inefficiencies.
How it works:
- Correcting running stride to improve efficiency
- Refining golf swing mechanics to avoid shoulder strain
- Optimising jump landing to protect knees in basketball or volleyball
Result: Better performance with reduced injury risk.
6. Boosting Recovery Through Advanced Modalities
Sports physiotherapy also uses modern therapeutic tools to speed recovery:
- Cryotherapy: Reduces swelling and pain
- Hydrotherapy: Improves circulation and joint movement
- Electrical stimulation (TENS/EMS): Relieves pain and strengthens muscles
- Shockwave therapy: Helps repair chronic injuries like tendonitis
These methods ensure athletes recover faster between training sessions and competitions.
7. Building Mental Resilience Through Education
Physiotherapy is not just physical; it’s psychological. Athletes often struggle with the frustration of injuries. Sports physiotherapists provide education, motivation, and structured recovery timelines, giving athletes confidence in their comeback.
Advantage: Improved focus, reduced stress, and a stronger mindset toward performance.
Key Areas of Sports Physiotherapy
1. Injury Prevention and Risk Reduction
- Biomechanical analysis
- Strengthening weak areas
- Sport-specific conditioning
2. Rehabilitation and Recovery
- Manual therapy
- Customised exercise programs
- Modalities like ultrasound, cryotherapy, or TENS
3. Performance Enhancement
- Flexibility training
- Core strengthening
- Endurance conditioning
4. Athlete Education
- Proper warm-up/cool-down routines
- Posture and technique guidance
- Nutrition and recovery advice
5. Return-to-Play Strategies
- Gradual progression plans
- Functional testing before competition
- Mental preparation support
Sports That Benefit Most from Physiotherapy
Running and Athletics
- Injury prevention for shin splints, IT band syndrome, and plantar fasciitis
- Performance improvements through stride correction and strength training
Football and Rugby
- Rehabilitation of ligament and hamstring injuries
- Strengthening for explosive power and agility
Tennis, Badminton, and Racquet Sports
- Shoulder stability and mobility exercises
- Wrist and forearm strengthening to reduce strain
Swimming
- Shoulder rehabilitation (rotator cuff injuries)
- Flexibility and mobility training for smoother strokes
Basketball and Volleyball
- Jump mechanics training to protect knees
- Ankle stability exercises to prevent sprains
Long-Term Benefits of Sports Physiotherapy
Sports physiotherapy is not just for the short term—it helps athletes build sustainable careers.
- Reduced injury downtime → more consistent training
- Improved biomechanics → long-term joint health
- Enhanced endurance and strength → better competition outcomes
- Confidence and resilience → stronger mental approach to performance
Insight: Athletes who integrate physiotherapy regularly, not only during injury phases, often extend their careers and achieve peak performance consistently.
When to See a Sports Physiotherapist
You should consult a physiotherapist if you experience:
- Persistent pain during or after exercise
- Repeated sports injuries
- Limited mobility or stiffness
- Decreased performance despite training
- Need for guidance on improving sport-specific techniques
Early intervention prevents small issues from becoming major injuries.
Conclusion
Sports physiotherapy is more than injury treatment; it’s a pathway to unlocking peak performance. By focusing on prevention, rehabilitation, biomechanics, and performance optimisation, physiotherapy empowers athletes to perform better, recover faster, and stay healthier for longer.
Whether you are an aspiring athlete or a seasoned professional, sports physiotherapy offers proven, science-backed benefits to enhance your physical abilities and protect your body from setbacks.
At Physio Asia Therapy Centre, we understand the unique demands athletes face. We are dedicated to providing efficient, effective, and evidence-based physiotherapy and rehabilitation services. Our expert physiotherapists design personalised sports recovery and performance plans tailored to your goals, helping you train harder, recover smarter, and perform at your very best.
Take the step toward better performance today- because in sports, every edge counts.